“We have the power to overcome this”
Calvin Vaughan, maintenance specialist, Facilities and Engineering
Years at YNHH: 17
“Not very much has changed in terms of the work I’m doing, except that now when we’re entering a COVID-19 area we have to put on all the personal protective equipment – the masks, face shields, gowns, etc.
Working in the COVID areas is part of the job. I know not everyone deals with things the same way, but I refuse to let this worry me. I’m a person of faith and a pastor. I trust God, and I trust that he’s made the doctors capable of taking care of the patients, and made us capable of taking care of ourselves.
I have so much respect when I see what the healthcare people are going through, I feel obligated to do my part, too. Sometimes, I’ll be working in an area where the patients are being difficult, and how the healthcare staff handle them is amazing. There are good people and bad; the people working here take care of them all, show them love and help them to be healed. That was true before COVID, too.
I don’t think we should let COVID-19 get the best of us. Sometimes challenges like this come to make us more focused, to remind us to love one another as people and to remind us what’s most important. We have the power to overcome this. The power is within ourselves.”
“My career has been built on commitment to my patients”
Wildine Felix, respiratory therapist
Years as a respiratory therapist: 17
“My day-to-day job has been changed in several ways, from basic protocol to the environment of the workplace. We routinely wear masks whether we are going into a patient’s room or charting; we wear masks when we’re among our coworkers; and we maintain the six-foot distance from each other to the best of our ability. Some of the equipment we use is now more essential than ever, such as HFNC (high-flow nasal cannulas) and ventilators. Because of this pandemic, we are more attentive to the vent count. Each day there is a new guideline, a new protocol and a new way of practice to adapt to. However, there is also a greater sense of camaraderie within the department and between disciplines as we all aim to provide the best care to each and every patient.
What motivates me is seeing a patient who was formerly intubated recover to the point where they are extubated and then discharged. We celebrate all the small and large victories at the hospital now. I'm proud to be part of a team of healthcare workers who can make a difference in our patients’ lives – a team of workers who care for each other in simple ways, such as ensuring each other’s PPE is secured. Another thing that motivates me is knowing that when I go home after a long day of work, my family, as always, is there to greet me. I have a great family support system at home that provides me with a sense of comfort and normalcy.
What scares me is the heightened sense of risking my life for the sake of others; however, that has always been a part of the healthcare mission. I am a strong woman, but being strong does not mean being without fears. Thankfully, I am able to control my fears rather than let them control me. I trust in the healthcare system; I trust in the PPE and the protocols and guidelines that are being bolstered every day. As a respiratory therapist, my career has been built on commitment to my patients. No pandemic can change that. We have worked with several diseases before and we will tackle other illnesses after.
These are sad times, but I feel comforted knowing that the entire world is thinking of all healthcare workers and finding ways to support us. I appreciate the thoughts and prayers of everyone. I get encouraging emails from members of my church, and I have called many friends several times to check on their well-being. It's almost like we all hang out more, virtually of course.
There are some positives that have come out of this crisis. More people are reaching out to one another in the world. We have all become a bit more empathetic and concerned. The workplace has become even more of a community. Now, everyone is vested in each other's well-being. I just thank God, who can bring light out of seemingly impossible situations.”
“This is a whole different level”
Cassie Graves, RN, SLA 2
Years as a nurse: less than 1
“Our floor was a surgical unit. Then we got a call that we would become a COVID floor. Our manager asked how we felt about it. I never hesitated. You can’t let your fear overcome the need for you to do your job. You have to do what you’re there to do for your patients. Someone has to do it – I’d rather it be me. I’m not afraid for myself. I’m just afraid I’ll get it and give it to my parents. There are patients in our unit who are in their 50s and 60s – my parents’ ages.
We’re doing a lot of jobs at once – we are doing all the vitals. We’re bringing food into the patient rooms. We’re cleaning the rooms and bringing out laundry and trash. No one else can go in.
You appreciate the teamwork even more now – you have to have a great team or it won’t work. With a limited amount of people going into the rooms, others are designated as runners to get anything we need. And you have to be more cautious and aware of what you are doing at all times. We’re getting more used to it now, but it was a huge change from how we used to do things. We had to learn how to do things in a whole new way. You have to adapt; it’s the only way to survive. That major change, combined with the fear of getting sick, is really overwhelming at times.
They teach you in nursing school what a pandemic is. You know it can happen but you don’t really think about it. I mean, I heard about Ebola and that kind of thing happening overseas, but it seemed so far away. This is a whole different level. This is real. You can actually see it.”
“These heroes make me want to show up every day”
Sandra Brooks, senior patrol officer, Protective Services
Time at YNHH: Nine months
“I wanted to share an experience I had at the SRC ED (Saint Raphael Campus Emergency Department) that really touched me. I was at the security desk when I saw a doctor come out into the empty waiting room and adjust his N95 mask. This is not a common occurrence, especially when the waiting room is empty. He appeared to need a tissue for a runny nose so I offered him a tissue. He declined the offer and blamed it on allergies, stating maybe a Sudafed would help. Being the caretaker type, and figuring the chances of him getting a Sudafed were slim, I offered him Claritin, which he also declined, making a joke that he is not happy unless he is complaining. He then disappeared back into the patient care area.
Moments later a nurse came out to the desk and was trying to tell me something but she was fighting tears. I had trouble understanding her and after hearing her say, ‘I’m going to cry, this just sucks,’ and then composing herself, she told me that a family member would be coming for a patient that was at end of life.
The family member did arrive for their short visit with their loved one. She was handled with loving care by the ED staff. I realized based on my observations that the doctor a short time before had also been upset and had likely come out to the waiting room area to take a minute to compose himself. I don’t know any other details but I do know that the nurse and doctor were grieving for a patient and family that they likely did not even know personally.
I am in awe of the medical staff and their tireless efforts to show up and do work that many would run from. Only the day before I observed a code on a COVID floor and watched the staff work their magic to a successful conclusion, soaked in sweat, but the team never missed a beat.
A few weeks back, my daughter was talking on the phone to her good friend, who works on one of the first COVID floors that opened on a Sunday evening. She told me her friend, who I also know very well, was going in to work on her night off because they were so short-staffed and they needed her. I’m a casual employee but these heroes make me want to show up every day for them so they can safely work through these unprecedented times. These are just a few of the many amazing things I observe on a daily basis here at YNHH.”
“I’m motivated by the opportunity I’ve been given”
Ana Mota, APRN, Yale Plastic Surgery/ MICU at SRC
“I have been a nurse in the MICU at SRC for five years. Last year, I graduated as an APRN and took on a new role working with Yale Plastic Surgery. Due to the COVID pandemic and elective surgeries being postponed, I volunteered to flex back to the MICU to help as an RN. I felt like this is where I belonged during this time, and I am appreciative of my manager, Lisa, and the entire plastic surgery team for being so supportive of this decision.
Returning to the ICU, I was surprised to see how different our day-to-day job was. Each morning, we gather our PPE into brown paper bags. Each time we leave a patient’s room, we must wipe down our face shields and replace our PPE in the paper bags, to be used throughout the day. ‘Running’ into patients’ rooms in urgent situations is a challenge, as we must gear up and remember to protect ourselves first – something that doesn't come naturally for nurses. Our policies on the use of PPE are also continuously changing. Providing patient care has changed, as we must carefully organize our day to cluster medications, blood work, etc.
The one thing that has stayed the same throughout all of this is the teamwork on the unit. We all work together. If one person has the full PPE attire on, that person will check on others to see if we're needed in different rooms prior to doffing.
I am coping by doing things I love on my days off. Exercising, reading, being outside. The sunny days make a big difference! I’m motivated by the opportunity I've been given to be back on the front lines alongside my team to fight this battle. I think the scariest part of all this is the fact that we don't have an end point. The unknown can be intimidating.
The biggest change in my life has been not seeing my family or friends since returning to the ICU. It's easy to feel isolated and alone at times, which is why I find staying productive around the house of great significance. I miss my loved ones very much, and I am looking forward to the days we can spend time together again.
The realities of the visitor restrictions have been a major challenge for patients, families, and those of us on the front lines. In order for families to see their loved ones, we set up Zoom meetings and hold an iPad up to the patient for them to communicate. Other times, I have held a phone on speaker for the chaplain to pray with the patient. I have stood in the room alone with the patient holding their hand while they’re being given their last rites by a priest over the phone. These experiences can be extremely difficult and heart-wrenching. I find myself forcing back tears, as I witness family sending words of encouragement to their critically ill family member, knowing they can't be physically present for them. I'm unsure when things will return to normal, or if we’ll have a completely new norm once this subsides. With all the chaos, I am proud and grateful to work alongside a team of resilient healthcare workers during this pandemic.”

Protective Services patrol officer Ken Ruge created a “wall of heroes” in the department featuring officers on the front line during the pandemic.
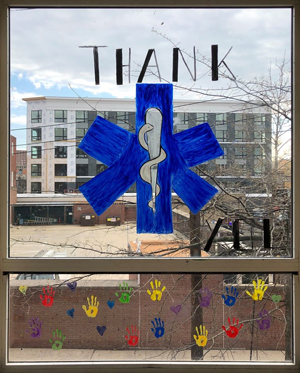
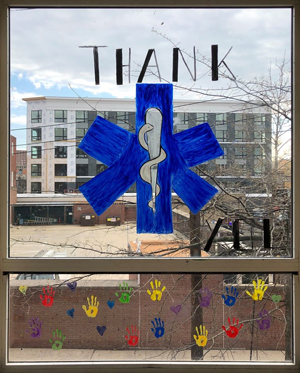
Patients, employees and community members are sharing thanks and encouragement via signs like this one, painted on a window at Yale New Haven Psychiatric Hospital by adolescent unit patients.
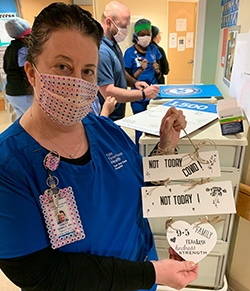
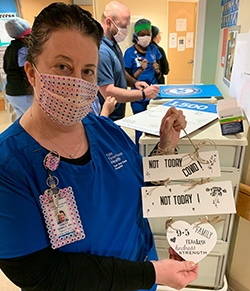
Tracey Demilo, RN, and her coworkers on EP 9-5 aren’t backing down from this fight.